Testosterone and Estradiol Pellet Therapy: A Modern Option for Hormone Optimization
For many men and women, low hormone levels can lead to frustrating symptoms like fatigue, weight gain, low libido, mood changes, and brain fog. Hormone replacement therapy (HRT) can be an effective way to restore balance and improve quality of life. One delivery method that has gained renewed popularity is subcutaneous hormone pellet therapy.
Pellets offer a convenient, long-lasting way to restore hormone levels without daily pills, patches, or creams. Here’s what you need to know.
A Brief History of Pellet Therapy
Hormone pellets are not new. In fact, pellet implantation has been used since the 1930s in both men and women. It was a common method in Europe and Australia for decades before falling out of favor in the United States when oral hormone tablets became more widely available and were heavily marketed by the pharmaceutical industry.
Interest in pellets has surged again in recent years as more patients and providers look for steady, physiologic hormone delivery without the fluctuations that can accompany other methods.
Several companies have popularized pellet therapy in the U.S., including BioTE, which is one of the largest and most widely recognized pellet therapy networks. BioTE provides standardized dosing protocols and training for providers, which has helped make pellet therapy more accessible and familiar to patients nationwide. While BioTE is not the only pellet system available, many patients first hear about hormone pellets through BioTE-related marketing or clinics.
How Pellet Therapy Works
Hormone pellets are tiny cylinders, about the size of a grain of rice, that contain either bioidentical testosterone. Estradiol pellets are even smaller, typically discs the same diameter as the testosterone, but only 1mm thick.
The Procedure
Pellets are inserted under the skin through a small incision—usually in the upper buttock, but they can also be placed in the flank or lower abdomen. The procedure is done in the office using local anesthesia and typically takes only a few minutes with minimal to no discomfort.
Once implanted, a capillary network forms around the pellets. The pellets slowly release hormones into the bloodstream over several months. The release is controlled by blood flow and cardiac output, so your body draws more hormone during times of increased activity and less when you’re at rest. This often results in stable, physiologic hormone levels without daily dosing.
Benefits of Hormone Pellet Therapy
Pellet therapy offers several unique advantages:
- Convenience – No daily pills, creams, or patches
- Steady hormone levels – Less fluctuation than some other delivery methods
- Bypasses the liver – No first-pass metabolism, which can reduce clotting risk compared to oral estrogen
- Symptom relief – Many patients experience improvements in energy, mood, libido, mental clarity, sleep, and overall well-being
- Long-lasting – Pellets typically last 2 1/2 –4 months in women and 4-6 months in men, depending on metabolism and activity levels and the type of strength of pellets used
One of the biggest advantages of pellet therapy is the stable, physiologic hormone levels it provides over time. Unlike weekly injections that create peaks and troughs, pellets deliver a steady release for months.
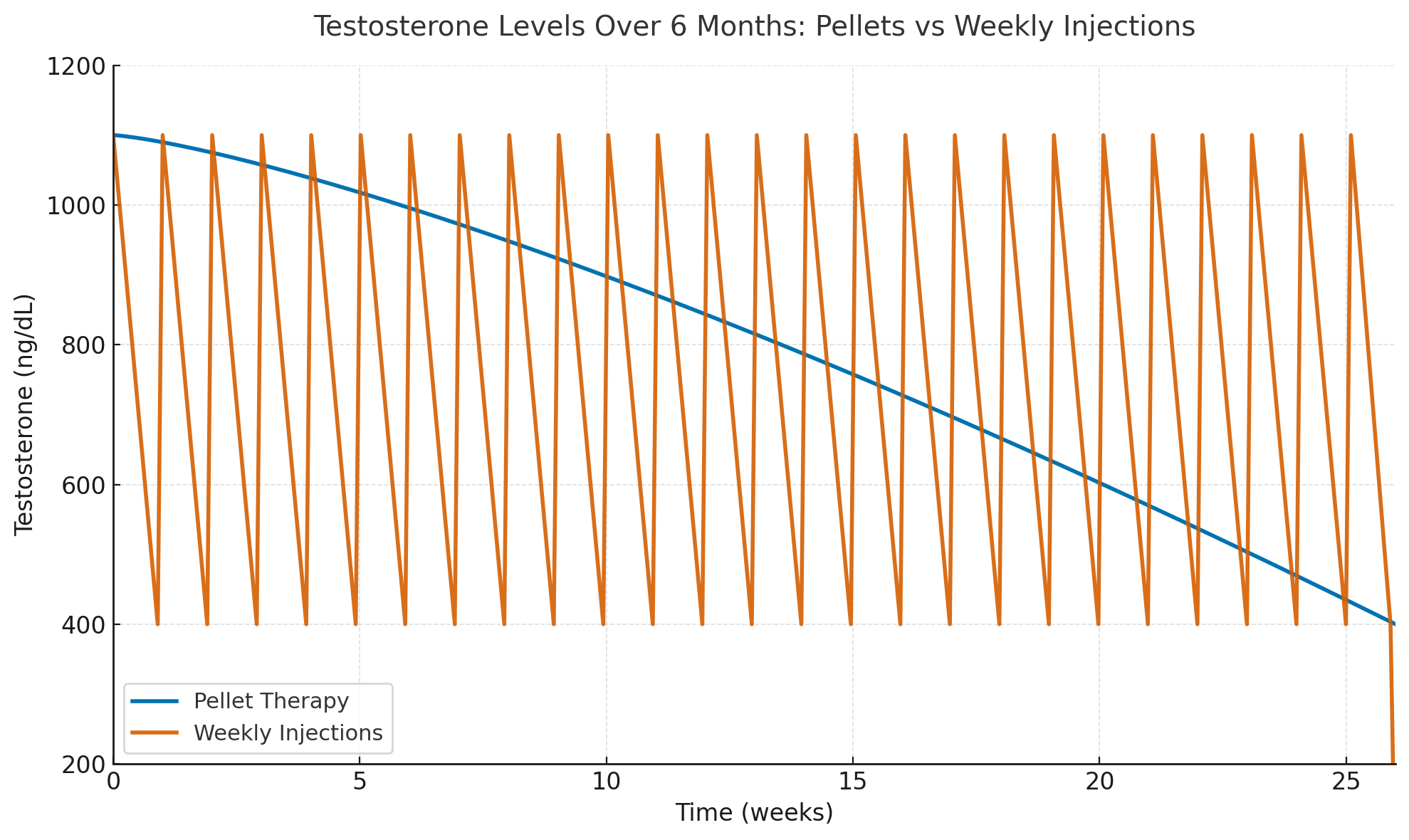
Graph: Testosterone levels over 6 months in men — Pellet therapy (blue) provides stable levels, while weekly injections (orange) create peaks and troughs between doses.
Who May Benefit
Pellet therapy can be an option for both men and women experiencing symptoms of hormone deficiency, such as:
- Fatigue or low energy
- Low libido or sexual dysfunction
- Mood changes, irritability, or depression
- Brain fog and difficulty concentrating
- Weight gain, loss of muscle mass, or reduced exercise tolerance
- Sleep disturbances
Candidates should undergo a thorough evaluation, including lab testing and review of medical history, to determine if pellet therapy is appropriate.
What About Women With a History of Breast Cancer?
For women with a personal history of hormone-receptor–positive breast cancer, estradiol pellets are contraindicated, since estrogen can stimulate breast tissue and potentially increase recurrence risk.
However, testosterone pellets may be an option in certain cases when combined with an aromatase inhibitor such as anastrozole, which blocks the conversion of testosterone into estradiol. This approach can help support energy, libido, mood, and overall well-being without significantly increasing estrogen exposure.
These decisions should always be made in collaboration with the patient’s oncology team and hormone therapy specialist, taking into account the type of breast cancer, treatment history, current medications, and individual goals.
Monitoring and Follow-Up
Regular follow-up and lab monitoring are essential.
There are 2 aspects of the treatment that are unique for each individual that need to be determined to get the optimal treatment results and minimal side effects:
- What dose of hormone is needed - A dosing calculator is typically used by the provider to determine the dose needed, but it is only a general guideline and may not be accurate for each person since everyone metabolizes hormones differently.
2. How often the procedure should be performed. The goal is to perform the next procedure before the levels drop so low that all of the initial symptoms have returned.
Labs are typically checked about 12 weeks after insertion in women to assess hormone levels and guide the timing of the next pellet placement. In men, the labs are typically checked around 5-6 months.
Many providers will check peak levels 4-6 weeks after the first procedure to ensure that the dosage of hormones is not too high.
Testosterone levels usually decline by around 3 months in women, 4-6 months in men.
Estradiol levels may remain elevated for up to 6 months or longer in some women.
Once the correct dose and timing of procedures has been determined, labs are only checked once or twice per year thereafter unless dosing changes are made.
This monitoring helps ensure safe, physiologic dosing and reduces the risk of over-replacement.
Understanding “Stacking” in Pellet Therapy
Because hormone pellets release their contents slowly over several months, it’s important to time repeat pellet insertions carefully. If a new pellet is placed before hormone levels from the previous pellet have fallen adequately, the hormones can “stack”—meaning the new dose is added on top of the residual hormone from the previous pellet.
Over time, stacking can lead to supraphysiologic hormone levels (higher than the body would naturally produce), which may increase the risk of side effects such as:
- Breast tenderness or swelling
- Fluid retention and bloating
- Mood swings or irritability
- Acne or increased hair growth
- Sleep disturbances or anxiety
- High estradiol or testosterone levels on labs
To prevent stacking, labs are drawn before repeating the procedure to make sure levels have dropped sufficiently before re-pelleting.
Proper timing, individualized dosing, and regular lab follow-up are key to avoiding stacking and maintaining safe, stable hormone levels over the long term.
Supporting Your Pellet Therapy: DIM, Vitamin D, B12, Ferritin, and Thyroid Testing
Hormone optimization works best when supported by other key factors that influence how hormones are metabolized and how you feel day-to-day.
DIM (Diindolylmethane)
DIM is a compound naturally found in cruciferous vegetables like broccoli and Brussels sprouts. Many providers recommend it as a nutritional supplement to support healthy estrogen metabolism, especially in patients receiving hormone therapy.
- Promotes beneficial estrogen pathways and helps reduce the conversion to more potent or potentially harmful estrogen metabolites.
- Has a mild aromatase-inhibiting effect, meaning it can slightly reduce the conversion of testosterone into estradiol.
- In women, this can support balanced hormone metabolism and reduce symptoms like breast tenderness.
- In men receiving testosterone pellets, DIM may help prevent excessive aromatization, which can lead to unwanted rises in estradiol, fluid retention, breast tenderness, or mood changes.
- Typically taken orally as a daily supplement and used as a natural adjunct to pellet therapy.
Note: DIM is not a replacement for prescription aromatase inhibitors when indicated (e.g., in breast cancer survivors), but it can be a valuable tool for fine-tuning estrogen metabolism in both women and men.
Vitamin D and Vitamin B12 Monitoring
Low vitamin D or vitamin B12 levels can mimic or worsen many of the same symptoms associated with hormone deficiency—such as fatigue, mood changes, cognitive fog, low energy, and muscle aches.
For that reason, vitamin D and B12 levels are routinely checked in our practice as part of hormone optimization.
- Vitamin D is essential for bone health, immune support, and hormone function.
- Vitamin B12 plays a key role in nerve health, red blood cell production, and mental clarity.
If deficiencies are found, appropriate supplementation is recommended to maximize the benefits of pellet therapy and address overlapping symptoms.
Ferritin Testing
Checking ferritin levels, which reflect the body’s iron stores, is an important part of evaluating women before starting pellet therapy.
Low ferritin is common in women, especially those with heavy menstrual cycles, and can cause symptoms such as:
- Fatigue and low energy
- Brain fog and difficulty concentrating
- Hair thinning or loss
- Low exercise tolerance
- Mood changes
These symptoms can overlap significantly with hormone deficiency. Additionally, low ferritin can impair how the body responds to testosterone, since adequate iron is needed for healthy red blood cell production and optimal cellular function. It can also suppress normal thyroid function because the thyroid gland needs iron in order to produce thyroid hormone.
Identifying and correcting low ferritin levels before or during hormone therapy can improve treatment effectiveness and help patients feel better faster.
Thyroid Function Testing
Thyroid disorders—especially hypothyroidism—can produce symptoms that closely mimic low testosterone, including:
- Fatigue and low energy
- Brain fog and difficulty concentrating
- Weight gain or difficulty losing weight
- Low libido
- Mood changes and depression
- Hair loss or thinning
Because of this overlap, it’s important to check thyroid labs before starting testosterone or estradiol pellets. If thyroid function is suboptimal, patients may not experience the full benefits of hormone therapy, or their symptoms may be mistakenly attributed to low testosterone when the thyroid is the primary issue.
Correcting thyroid dysfunction first—or at least identifying and co-managing it—ensures that pellet therapy is targeted, effective, and not masking another underlying hormonal problem.
Potential Side Effects
Pellet therapy is generally well tolerated, but possible side effects include:
- Temporary tenderness or bruising at the insertion site
- Acne or increased hair growth (usually mild)
- Fluid retention or breast tenderness (more common with higher estradiol levels)
- Rare pellet extrusion (pellet working its way out through the incision)
- Infection at the insertion site. Since most providers perform the procedures under sterile conditions, this is extremely rare
Serious complications are uncommon when pellets are placed by experienced providers and followed appropriately.
Of note, it is important to keep the incision area clean and dry after the procedure. In women, we recommend that they keep the steri-strip on the incision, avoid soaking in water, and avoid gluteus exercises (squats, lunges, etc) for 3 days after the procedure. In men, we recommend keeping the bandage in place, avoid soaking in water, and avoid gluteus exercises for 1 week.
BTW, the gluteus exercise precautions only apply if you had the pellets inserted in your buttock area. Flank and abdominal insertions do not have that precaution.
Typical Costs
While pricing varies by practice and location, typical costs are around $350 per procedure for women and $700–$750 for men, plus the cost of periodic lab work. Because pellets last several months, this compares favorably with the cumulative cost of other hormone delivery methods over time such as shots and creams.
Pellet Therapy vs Other Delivery Methods
Pellets are one of several hormone delivery options. Others include:
- Transdermal patches, creams, or gels
- Oral formulations
- Injections
- Vaginal delivery - creams and troches
Pellets stand out for their convenience and stable hormone delivery, but they aren’t adjustable after placement.
For someone with a history of sensitivity to medications or even small dosage changes, pellets may not be the best first option. Once pellets are inserted, it will be 3-6 months before dosing changes can be made. It may therefore be better to start with creams, patches or shots in those individuals. If a stable dose is found and they are tolerating the other modalities, switching to pellets later may be a good option.
Is Pellet Therapy Right for You?
Hormone pellet therapy can be a powerful tool for restoring optimal hormone balance, especially for patients who want a “set it and forget it” approach. But it’s not the best choice for everyone.
The ideal candidate is someone who:
- Has documented hormone deficiency and symptoms
- Wants a low-maintenance option
- Can commit to follow-up labs and visits
- Understands the risks and benefits of long-acting therapy
Schedule a Hormone Consultation
If you’re curious about hormone pellet therapy and whether it might be right for you, I can help.
👉 Schedule a hormone consultation to learn more and get personalized guidance.
References
- Glaser R, et al. Subcutaneous hormone pellet implants for hormone replacement therapy in women: safety and efficacy. Maturitas. 2013;74(4):357–362.
- The North American Menopause Society. 2022 Hormone Therapy Position Statement. Menopause. 2022;29(7):767–794.
- Davison SL et al. Androgen levels in adult females: changes with age, menopause, and oophorectomy. J Clin Endocrinol Metab. 2005;90(7):3847–3853.
4. Stuenkel CA et al. Treatment of symptoms of the menopause: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2015;100(11):3975–4011.

