Acetaminophen & Pregnancy: A Balanced Perspective
Introduction
Acetaminophen (Tylenol®) has long been considered the “go-to” medication for pain and fever relief during pregnancy. Doctors often recommend it as the safest option compared to NSAIDs or aspirin. But emerging research suggests that acetaminophen may not be as risk-free as once believed—especially during pregnancy.
Is this concern real or overblown? Let’s look at the controversy and the research behind it…
How Acetaminophen Works and Why It Matters in Pregnancy
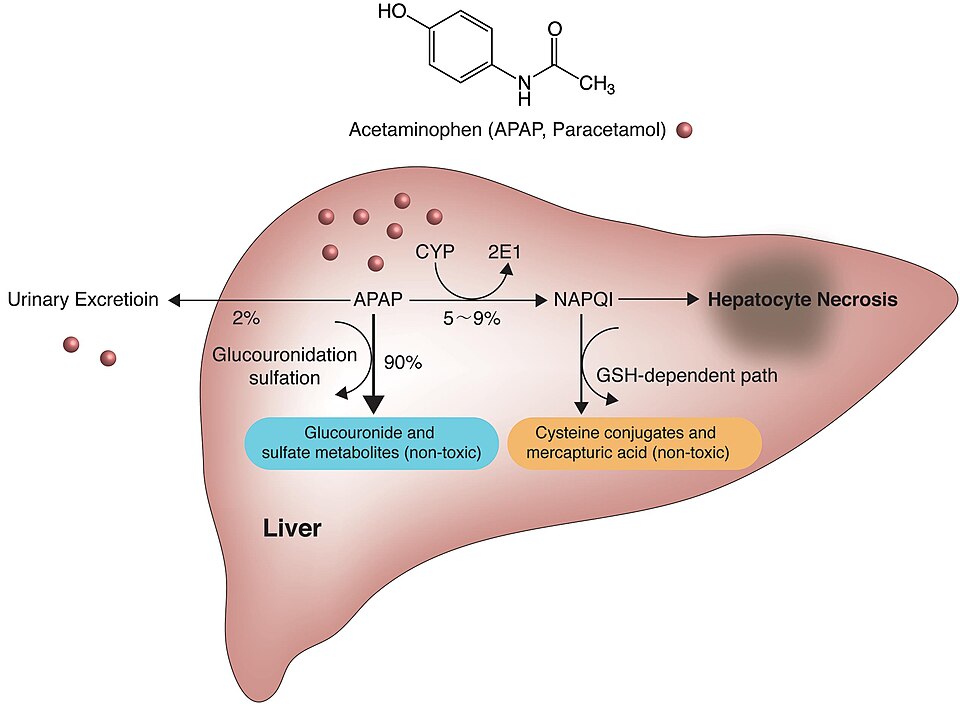
Acetaminophen reduces pain and fever by acting on the brain’s pain and temperature centers. However, it comes at a biochemical cost. When metabolized in the liver, it produces a toxic byproduct called NAPQI. Normally, NAPQI is neutralized by glutathione, one of the body’s most important antioxidants.
But here’s where the potential problem arises:
- Pregnancy already increases oxidative stress and detox demand¹.
- Glutathione levels are naturally lower during pregnancy².
- Acetaminophen depletes glutathione even further³.
This creates a situation where both mom and baby may be more vulnerable to oxidative stress and toxin buildup.
Research Linking Acetaminophen and Pregnancy Risks
Several large studies have found associations between prenatal acetaminophen use and:
- Increased risk of ADHD and autism spectrum disorders in children⁶⁷.
- Altered reproductive development in boys, including cryptorchidism (undescended testes)⁸.
- Increased childhood asthma and wheezing⁹.
While these studies do not prove causation, they raise concern—especially when combined with biological vulnerabilities. From a scientific perspective, it makes sense that compromised detoxification capacity could magnify these risks.
Of note, there have been several studies that have not shown a link between acetaminophen and autism. The most recent is an article in JAMA from 2024. Click here to see the study.
The FDA’s New Recommendations — and the Pushback
Recently, the FDA and other regulatory bodies have begun issuing more cautious statements about acetaminophen use in pregnancy. They acknowledge the body of evidence potentially linking acetaminophen exposure to developmental and reproductive risks. Some recommendations include:
- Using the lowest effective dose for the shortest possible duration.
- Avoiding repeated or prolonged use during pregnancy.
- Encouraging more research into genetic vulnerabilities.
Why Conventional Medicine is Frustrated
The conventional medical community has expressed strong pushback to these recommendations. Here are their valid arguments:
- Evidence threshold: Doctors argue the current studies show correlation but not causation, and they fear patients will panic unnecessarily. Correlation means 2 things are associated or happen together. For example, children who eat more ice cream also tend to have more sunburns. Ice cream doesn’t cause sunburn - it’s just that both happen more often in the summer. Causation means one thing directly leads to another. For example, drinking alcohol in large amounts can cause liver damage. The alcohol directly harms the liver, and repeated exposure increases the likelihood of developing cirrhosis.
At this point, we don’t know definitively if acetaminophen is a direct cause of things such as autism or if it is just correlated because acetaminophen is about the only medication for pain or fever that has been recommended for pregnant women.
- Clinical experience: For decades, acetaminophen has been the “least bad” option during pregnancy compared to NSAIDs or opioids. Removing it leaves few alternatives for pregnant women when they have pain and/or fever.
- NSAIDs are proven to be dangerous in pregnancy: Nonsteroidal anti-inflammatory drugs (ibuprofen, naproxen, aspirin in high doses) are clearly associated with pregnancy complications. Studies have linked NSAID use—especially in the third trimester—to premature closure of the ductus arteriosus in the fetus, oligohydramnios (low amniotic fluid), miscarriage, and impaired kidney development¹²¹³. Because these dangers are well-established, most guidelines advise avoiding NSAIDs during pregnancy altogether. These risks have left acetaminophen as the only “default” medication.
- Concerns of Untreated High Fever: Physicians worry that if pregnant women avoid acetaminophen completely, untreated fevers (especially in the first trimester) could pose a greater risk to fetal development than the medication itself. For example, this article showed evidence that fever itself can increase the risk of developing autism. By the way, this is for a true fever (>100.4° Fahrenheit). A temperature <100.4° may make you feel crummy, but it doesn't meet the scientific definition of fever.
- Medicolegal implications: Changing recommendations may expose providers to liability for past prescribing practices. If we find that acetaminophen does indeed increase the risk for autism and ADHD, are all of the doctors that have recommended using it during pregnancy at risk for massive lawsuits?
I was a fully conventional medicine doctor for over 20 years. I entered into the functional medicine world beginning in 2019. I am no longer a conventional medicine doctor, but I am also not fully a functional medicine doctor either. Both camps have their strengths and weaknesses. I believe it is important to look at both sides of that coin and try to see where the truth lies, which is often somewhere in the middle. That is what I am attempting to do in this article.
Conventional medicine can be very stubborn and will often wait for irrefutable proof before acting on new research or findings. Many in the conventional world will attack different viewpoints if it is different from the accepted standard of care. One example is cigarette smoking: for decades, despite mounting observational evidence of harm, the medical establishment resisted warnings about the dangers of tobacco use until long-term, large-scale studies left no room for doubt. Millions suffered in the meantime.
On the other hand, functional/integrative medicine attempts to emphasize early precaution and prevention, looking for root causes of illness. While this is a strength, it can also be a weakness. Sometimes, the eagerness to act before all the evidence is in leads to unproven or even unsafe treatments. For instance, high-dose intravenous hydrogen peroxide therapy has been promoted in some alternative medicine circles as a cure-all, despite lacking evidence and carrying significant risks of tissue damage and embolism.
Both extremes have pitfalls. The best path forward is to learn from each side—balancing caution and prevention with solid evidence and safety.
Could an MTHFR Mutation Increase the Risk?
There is growing concern that methylation issues could increase the risk of the development of conditions such as autism. The MTHFR gene (methylenetetrahydrofolate reductase) plays a key role in the body’s methylation cycle, which is essential for:
- Converting dietary folate into its active form.
- Supporting DNA synthesis and repair.
- Detoxifying homocysteine.
- Recycling antioxidants such as glutathione⁴⁵.
Two common variants of MTHFR—C677T and A1298C—can reduce the enzyme’s activity by up to 70%⁴. This reduction can have significant consequences, especially during pregnancy:
- Impaired methylation capacity → less efficient DNA repair and gene regulation.
- Elevated homocysteine → associated with increased risk of preeclampsia, miscarriage, and neural tube defects⁵.
- Reduced glutathione recycling → less ability to neutralize oxidative stress and toxins¹¹.
What This Could Mean for Pregnancy
- Greater vulnerability to oxidative stress in both mother and baby.
- Potential amplification of risks already suggested in studies, such as ADHD, autism, and reproductive development issues⁶⁷⁸.
- Higher nutrient demands for folate, B12, B6, and antioxidants to support detox pathways.
From a functional medicine standpoint, the MTHFR-acetaminophen connection is important because it suggests not all women face equal risk. Genetic testing for MTHFR and monitoring homocysteine levels can provide useful insight into whether acetaminophen use could be more problematic during pregnancy.
The Role of Leucovorin
Mothers with MTHFR variants and other causes of decreased methylation often need more than standard prenatal vitamins. That’s where leucovorin (folinic acid) can play a role.
- Folinic acid is a bioactive form of folate that bypasses the MTHFR enzyme¹⁰.
- It provides a direct pathway for DNA synthesis and methylation, even when MTHFR activity is reduced.
- Unlike folic acid (which requires MTHFR conversion), folinic acid can be efficiently used by the body.
Why This Matters in Pregnancy:
- Supports neural tube development and reduces risk of birth defects such as spina bifida.
- Helps maintain methylation pathways under stress.
- Provides better support for glutathione recycling, which is especially important when acetaminophen depletes antioxidant stores¹¹.
For many women with MTHFR variants, a combination of methylfolate and folinic acid (leucovorin) provides broader coverage than either alone.
Strategies to Consider to Reduce Risk
If you feel that completely avoiding acetaminophen isn’t realistic, here are some middle-ground approaches to lower potential risk:
- Reserve use for true need – don’t take it “just in case” for minor aches. Save it for significant fever or pain where benefits outweigh risks.
- Use the lowest effective dose – don’t exceed 500–650 mg at a time unless specifically directed by your physician.
- Limit duration – avoid daily or prolonged use. Occasional, short-term use is far safer than chronic intake.
- Support detox pathways – ensure you’re on a prenatal with methylfolate and/or leucovorin, plus antioxidants (vitamin C, NAC, selenium) to help preserve glutathione.
- Monitor fever carefully – untreated high fevers can also be dangerous for the baby. The goal is balance, not rigid avoidance.
- Consider testing – ask about being tested for MTHFR variants and homocysteine levels. If you are negative for MTHFR and your homocysteine is low (<10 µmol/L), your risk for potential acetaminophen-related issues is likely lower.
These compromises don’t remove risk completely, but they can meaningfully reduce it while giving mothers and providers some flexibility in managing symptoms during pregnancy.
Hopefully, further research on this topic will clarify true risks and recommendations that should be followed.
Conclusion
Acetaminophen has long been considered to be “safe” in pregnancy, but the fact is, we don’t really know. Some studies have suggested an increased risk for autism and ADHD while others have not⁶⁷
The combination of increased glutathione depletion³ and reduced methylation capacity⁴⁵ could potentially raise the risk of complications for both mother and baby.
The FDA’s new cautionary stance highlights the growing awareness of these risks. Yet the strong pushback from conventional medicine reflects the tension between waiting for certainty versus acting with precaution. Public health officials have chosen to inform the population of the possible link, even if it's not a settled issue. It's up to each individual to consider the information and make your own decision.
A Plea for Open-Mindedness
In closing, I encourage everyone to remain open-minded and research the information for themselves. Don’t allow politics or the personal dislike of a public figure to taint our ability to make informed decisions. Health decisions—especially those affecting pregnancy and the next generation—deserve to be made with clarity, curiosity, and an honest evaluation of the evidence on both sides.
References
- Burton GJ, Jauniaux E. Oxidative stress in pregnancy. Placenta. 2011;32 Suppl 2:S66–S69.
- Castillo RL et al. Maternal plasma glutathione and oxidative stress markers during pregnancy. Clin Chim Acta. 2019.
- James LP et al. Mechanisms of acetaminophen hepatotoxicity and their translation to the human pathophysiology. Clin Liver Dis. 2015.
- Frosst P et al. A candidate genetic risk factor for vascular disease: a common mutation in methylenetetrahydrofolate reductase. Nat Genet. 1995.
- Stover PJ. One-carbon metabolism–genome interactions in folate-associated pathologies. J Nutr. 2009.
- Ji Y et al. Association of cord plasma acetaminophen metabolites with attention-deficit/hyperactivity disorder. JAMA Psychiatry. 2020.
- Avella-Garcia CB et al. Acetaminophen use in pregnancy and neurodevelopment: A systematic review and meta-analysis. Int J Epidemiol. 2016.
- Kristensen DM et al. Intrauterine exposure to acetaminophen and male reproductive function. Endocrinology. 2011.
- Shaheen SO et al. Prenatal paracetamol exposure and risk of asthma and elevated IgE in childhood. Clin Exp Allergy. 2005.
- Bailey SW, Ayling JE. The extremely slow and variable activity of dihydrofolate reductase in human liver. Proc Natl Acad Sci USA. 2009.
- James SJ et al. Metabolic biomarkers of increased oxidative stress and impaired methylation capacity in children with autism. Am J Clin Nutr. 2004.
- Koren G, Florescu A, Costei AM, Boskovic R, Moretti ME. Nonsteroidal anti-inflammatory drugs during third trimester and the risk of premature closure of the ductus arteriosus: A meta-analysis. Ann Pharmacother. 2006.
- Nakhai-Pour HR, Broy P, Sheehy O, Bérard A. Use of nonaspirin NSAIDs during pregnancy and the risk of spontaneous abortion. CMAJ. 2011.

